You got your sleep test results back and now you’re staring at confusing numbers. AHI, RDI, oxygen saturation, sleep stages. What does any of this mean for your health? Most people have no idea how to make sense of these medical reports.
Dr. Elaine Wu at ReNEW Dental, trained at Boston University and the Kois Center, helps patients understand their sleep study results. This guide breaks down each key metric in plain English, shows what your numbers mean, explains common mistakes, and gives clear action steps so you can move forward confidently.
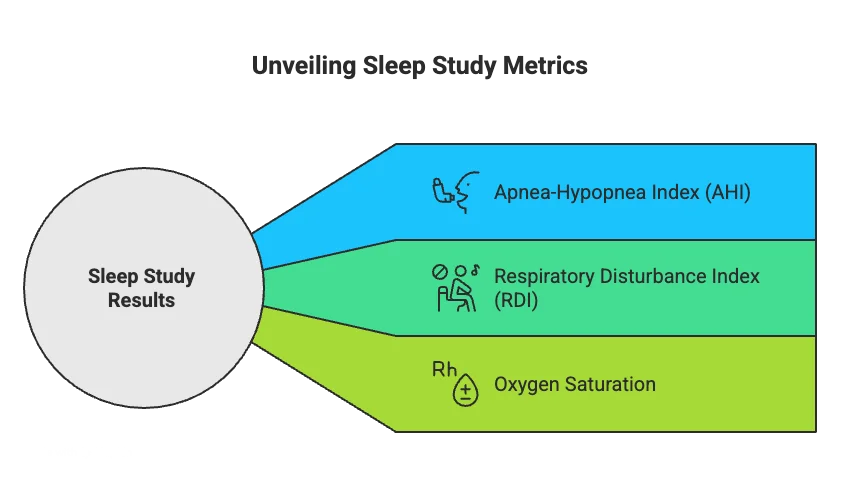
What Sleep Study Results Measure
Sleep studies track specific things happening in your body while you sleep. The numbers tell a story about your breathing, oxygen levels, and sleep quality.
AHI stands for Apnea-Hypopnea Index. It counts how many times per hour you stop breathing or your breathing gets too shallow. Under 5 is normal. Between 5 and 15 means mild sleep apnea. From 15 to 30 is moderate. Over 30 is severe.
RDI means Respiratory Disturbance Index. It’s similar to AHI but includes more breathing problems. It counts complete stops plus partial blockages plus times when breathing effort increases enough to wake you slightly. Oxygen saturation shows the percentage of oxygen in your blood. Normal people stay above 90 percent all night.
Understanding Your Specific Numbers
Your sleep study report includes several measurements that work together. Each number provides a different piece of the puzzle.
Sleep stages show how much time you spent in light sleep, deep sleep, and REM sleep. Adults need about 20 to 25 percent REM sleep. Deep sleep should be around 13 to 23 percent. If these numbers are way off, something kept interrupting your natural sleep cycles.
Arousals count how many times you partially woke up during the night. Fewer than 15 per hour is normal. More than that means something kept disturbing your sleep. Sleep apnea causes lots of arousals because your brain has to wake you up to start breathing again.
Body position matters too. Some people only have breathing problems when sleeping on their back. Your report might show your AHI is 8 overall but jumps to 25 when you’re on your back. Home tests are convenient and cheaper but can miss mild cases. Lab tests catch everything but cost more.
Key Differences Between Sleep Test Types
Understanding which test you had helps you know how accurate your results are. Each type has strengths and limitations.
| Test Type | What It Measures | Accuracy | Best For |
| Home Sleep Test | Breathing, oxygen, heart rate | 70-80% accurate | Moderate to severe cases |
| Lab Polysomnography | Brain waves, breathing, oxygen, movements | 95%+ accurate | All severity levels |
| WatchPAT Device | Peripheral arterial tone, oxygen, heart | 85-90% accurate | Mild to moderate cases |
| Overnight Oximetry | Only oxygen levels | Limited | Initial screening only |
Home tests work great if you have obvious symptoms and moderate to severe apnea. They might miss mild cases. Lab tests catch everything but cost more.
If your home test comes back negative but you still have symptoms, ask about a lab test. False negatives happen.
From Data to Diagnosis
Raw numbers become a diagnosis when a sleep specialist reviews everything together. They consider your symptoms, health history, and all the measurements.
Mild obstructive sleep apnea means AHI between 5 and 15. This might need treatment depending on your symptoms and health risks. Moderate sleep apnea ranges from 15 to 30 events per hour. Most doctors recommend treatment at this level. Your oxygen is dropping too often.
Severe sleep apnea means over 30 events per hour. Some people hit 60 or even 100. This requires treatment right away. Your body is under serious stress all night. Health risks go way up at this severity level.
Your Next Steps After Getting Results
Results are just the beginning. What you do next makes the biggest difference.
Schedule a follow-up with a sleep specialist. They’ll explain what your numbers mean. They’ll recommend treatment options that fit your situation. Ask specific questions about your results.
Consider lifestyle changes regardless of severity. Losing weight helps if you’re overweight. Avoiding alcohol before bed reduces breathing problems. Sleeping on your side can cut events in half.
Start tracking your symptoms daily. Note how tired you feel, morning headaches, mood changes. This helps your doctor see if treatment is working.
Common Questions and Concerns About Results
Test anxiety and poor sleep during the study concern many people. You tossed and turned all night. Does that mean results are useless? Usually not. Even partial sleep data shows patterns.
Movement affects numbers but doesn’t invalidate results. The test captures what actually happens when you sleep. Medication effects matter for some drugs. Tell your doctor what you take.
When Results Don’t Match How You Feel
Sometimes objective numbers and subjective experience don’t line up. This creates confusion.
You might have mild AHI but feel terrible every day. Other factors could be making things worse. Depression, thyroid problems, or other sleep disorders might be layering on top.
High AHI but you feel fine seems backwards. Some people adapt to poor sleep. That doesn’t mean the apnea isn’t hurting them. Heart damage still develops silently. Treatment prevents future complications.
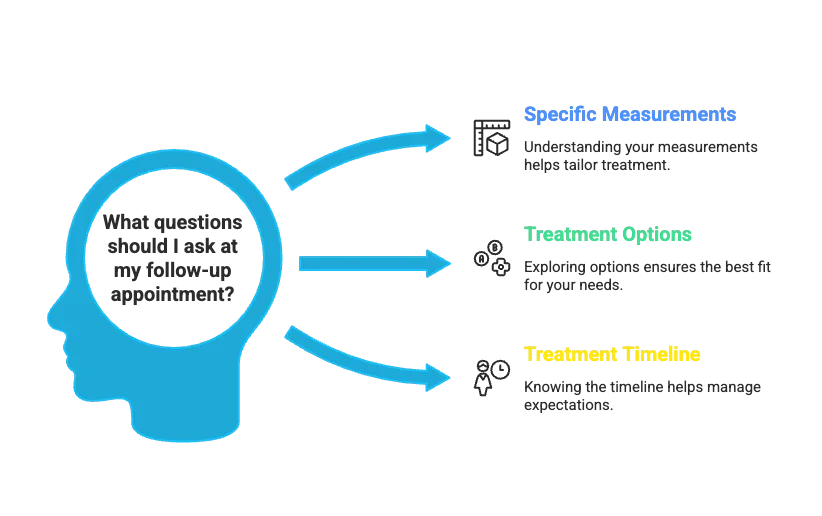
Important Things to Discuss at Your Follow-Up
Bringing the right questions to your appointment gets you better answers.
Questions about your specific measurements. Which number is most concerning. Did the test catch everything? What’s causing my breathing to stop? Are there other sleep disorders we should check for. How quickly do I need treatment?
Questions about treatment options. What treatments work best for my severity level. Can lifestyle changes help or do I need medical treatment? What if I can’t tolerate CPAP. Are oral appliances an option? How long until treatment helps.
Your doctor should answer everything clearly. If they rush through explanations, ask them to slow down.
How Treatment Changes Future Results
Follow-up testing shows if treatment works. Most people do another sleep study after starting treatment. Comparing before and after numbers proves effectiveness.
CPAP therapy should drop your AHI close to zero if working properly. If your AHI stays above 5 on CPAP, something needs adjustment. Maybe pressure settings are wrong. Maybe the mask doesn’t fit right.
Oral appliance therapy typically reduces AHI by 50 to 70 percent in appropriate cases. Dr. Wu uses custom oral appliances to reposition your jaw and keep your airway open. Follow-up testing confirms the appliance is working.
Your Path Forward with Confidence
Understanding your sleep study results removes the mystery and anxiety. You know what the numbers mean. You know what questions to ask. You know what actions to take next.
Dr. Elaine Wu at ReNEW Dental, with her training from Boston University and the Kois Center, specializes in helping patients understand their sleep apnea diagnosis. She provides expert treatment with custom oral appliances and creates personalized treatment plans addressing your specific needs.
Don’t let confusing medical jargon stop you from getting help. Your sleep quality affects everything in your life. Schedule your consultation with Dr. Wu at ReNEW Dental today to discuss your sleep study results and discover effective treatment options.
ReNEW Dental
978-451-1500
1201 Main St. Tewksbury, MA 01876
Schedule your consultation today!
Frequently Asked Questions
What does an AHI of 15 mean for my health?
An AHI of 15 means you stop breathing 15 times per hour during sleep. This falls into moderate sleep apnea category. Your oxygen levels are dropping repeatedly throughout the night. Most sleep specialists recommend treatment at this level.
American Academy of Sleep Medicine guidelines classify AHI 15-30 as moderate and recommend therapeutic intervention. National Heart, Lung, and Blood Institute research shows untreated moderate sleep apnea increases cardiovascular disease risk.
How accurate are home sleep tests compared to lab studies?
Home sleep tests are 70 to 80 percent accurate for moderate to severe sleep apnea but can miss mild cases. Lab polysomnography is 95 percent accurate because it measures brain waves, breathing, oxygen, and movements simultaneously. If your home test is negative but symptoms continue, request a lab study. Sleep Foundation research shows home tests work well for straightforward cases but laboratory testing remains the gold standard.
Mayo Clinic guidelines recommend lab testing when home results are inconclusive.
What should I do if my results show borderline sleep apnea?
Borderline results with an AHI between 4 and 6 require discussion with a sleep specialist about your symptoms and risk factors. Even mild numbers warrant treatment if you have daytime sleepiness or high blood pressure. Start with lifestyle changes like weight loss, side sleeping, and avoiding alcohol before bed.
Johns Hopkins sleep medicine research shows symptom severity matters as much as AHI numbers for treatment decisions. American Academy of Dental Sleep Medicine recommends considering oral appliance therapy for mild cases when symptoms affect quality of life. ADA Source
Related Articles
Common Sleep Apnea Treatments – Positional Therapy – Oral Appliance Therapy – Signs of Sleep Apnea – Sleep Apnea Comorbidities – Sleep Apnea Testing




